SOAP notes are a key tool in speech and language therapy, helping therapists document patient progress, create treatment plans, and communicate effectively with other healthcare professionals. If you’re new to writing SOAP notes or looking to refine your approach, this guide will walk you through everything you need to know.
What Are SOAP Notes?
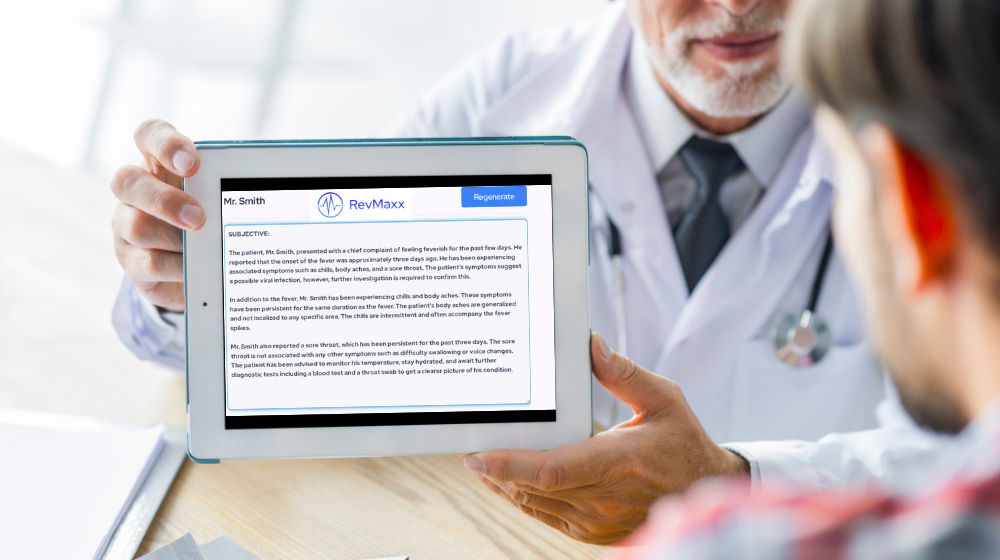
SOAP notes are a method of documentation used by healthcare providers to track a patient’s progress during treatment. SOAP stands for Subjective, Objective, Assessment, and Plan, each representing a section of the note that focuses on different aspects of the patient’s session.
Why SOAP Notes Matter in Speech and Language Therapy
In speech and language therapy, SOAP notes are essential for keeping an accurate record of a patient’s progress, challenges, and the strategies used to overcome them. These notes help therapists stay organized, ensure continuity of care, and make it easier to communicate with other healthcare professionals involved in the patient’s care.
Breaking Down the SOAP Format
Subjective (S)
The Subjective section is where you record the patient’s or caregiver’s perspective on the patient’s condition. This might include how the patient feels, any concerns they have, or changes they’ve noticed in their speech or language abilities. For instance, a patient might mention they’re struggling with word retrieval during conversations, which is valuable information for guiding treatment.
Objective (O)
The Objective section is focused on observable and measurable data. This could include the results of assessments, specific behaviors noted during the session, or progress in achieving therapy goals. For example, you might document that the patient successfully completed a speech exercise with 80% accuracy, a quantifiable measure of progress.
Assessment (A)
In the Assessment section, you’ll interpret the information gathered in the Subjective and Objective sections. This is where you analyze the patient’s progress, identify patterns, and make a clinical judgment about the effectiveness of the current treatment plan. The Assessment is crucial for determining the next steps in therapy.
Plan (P)
The Plan section outlines the next steps in the patient’s treatment. This might include continuing current strategies, introducing new exercises, or modifying goals based on the patient’s progress. A well-defined plan ensures that both the therapist and patient are clear on what needs to be done next.
Advantages of Using SOAP Notes
Improving Communication Among Professionals
SOAP notes speech and language provide a standardized format that makes it easier for healthcare professionals to understand and share patient information. Whether you’re collaborating with a doctor, occupational therapist, or another speech-language pathologist, SOAP notes ensure that everyone is on the same page.
Enhancing Patient Care and Treatment Planning
By consistently documenting patient progress and adjusting treatment plans accordingly, SOAP notes help ensure that patients receive the most effective care. Regularly reviewing these notes allows therapists to make informed decisions that enhance the quality of treatment.
Ensuring Legal Compliance and Protection
Accurate SOAP notes are vital for legal compliance. They provide a clear record of the care provided, which can be crucial in case of audits or legal disputes. Proper documentation demonstrates that the therapist has met their professional responsibilities and provided appropriate care.
Step-by-Step Guide to Writing Effective SOAP Notes
Preparing Before You Write
Before you begin writing a SOAP note, gather all the necessary information from the session, including any assessments, observations, and feedback from the patient or caregiver. Having everything organized will make the writing process smoother and more efficient.
Crafting the Subjective Section
Start your SOAP note with the Subjective section. Record the patient’s or caregiver’s statements about the patient’s condition. Be sure to capture their exact words when possible, as this can provide important context for understanding their concerns.
Detailing the Objective Observations
Next, move on to the Objective section. Here, you’ll document any observable data, such as test scores, specific behaviors, or measurable outcomes from the session. This section should be factual and free from interpretation.
Interpreting the Assessment
In the Assessment section, analyze the information you’ve gathered. Discuss the patient’s progress, any challenges they’re facing, and how effective the current treatment plan is. This is where you’ll make a clinical judgment about what’s working and what might need to change.
Formulating a Clear Plan
Finally, outline the Plan for the next steps in treatment. Be specific about what will happen next, whether that’s continuing with the current approach, introducing new techniques, or setting new goals. The Plan should be actionable and directly tied to the insights gained from the Assessment.
Common Pitfalls to Avoid in SOAP Notes
Including Too Much or Too Little Information
One common mistake is overwhelming the SOAP note with too much detail or, conversely, not including enough information. Aim for a balance where you provide enough detail to be clear and informative but avoid unnecessary complexity.
Being Vague or Ambiguous
Clarity is crucial in SOAP notes. Avoid vague language that could be interpreted in multiple ways. Be as specific as possible, especially in the Objective and Plan sections, to ensure that your notes are useful to other professionals.
Relying Too Heavily on Subjective Opinions
While the Subjective section is important, don’t let it dominate your note. The Objective, Assessment, and Plan sections should be based on measurable data and professional judgment rather than personal opinions or feelings.
Case Example: Writing a SOAP Note for Speech and Language Therapy
Subjective: Understanding the Patient’s Experience
“Patient reports difficulty finding the right words during conversations, especially when speaking with strangers. Feels frustrated and anxious about social interactions.”
Objective: Recording Observable Data
During the session, the patient exhibited word-finding difficulties in 40% of spontaneous speech attempts. Successfully completed word retrieval exercises with 75% accuracy.
Assessment: Analyzing the Information
The patient’s word-finding issues appear to be exacerbated by anxiety, particularly in unfamiliar social situations. Continued focus on vocabulary expansion and anxiety management is recommended.
Plan: Outlining the Next Steps
Continue current therapy with an emphasis on word retrieval exercises and introduce relaxation techniques to manage anxiety. Reevaluate progress in four weeks.
Integrating SOAP Notes with Goal Setting
Setting SMART Goals Based on SOAP Data
SMART (Specific, Measurable, Achievable, Relevant, Time-bound) goals are essential in speech and language therapy. Use the information from your SOAP notes to set clear, actionable goals that align with the patient’s needs and progress.
Monitoring Progress with SOAP Notes
SOAP notes provide a framework for tracking the patient’s progress toward their goals. Regularly reviewing these notes allows you to see how well the patient is meeting their objectives and whether any adjustments are needed.
Adjusting Goals as Needed
As the patient progresses, their goals may need to be adjusted. Use your SOAP notes to guide these changes, ensuring that goals remain relevant and achievable as the patient’s abilities improve.
Best Practices for SOAP Notes in Speech and Language Therapy
Consistency is Key
Consistency in your SOAP notes is vital for tracking progress and ensuring continuity of care. Stick to the same format and level of detail in each session to make it easier to compare notes and monitor changes over time.
Keep it Clear and Concise
Clear and concise documentation is more effective and easier for others to understand. Avoid jargon or overly complex language, and focus on providing the essential information in a straightforward manner.
Use Professional Language
While clarity is important, remember that SOAP notes are a professional document. Use proper grammar and spelling, and maintain a professional tone throughout.
How to Use SOAP Notes with Electronic Health Records (EHR)
Benefits of EHR Integration
Integrating SOAP notes with Electronic Health Records (EHR) can streamline the documentation process, making it easier to store, access, and share information. EHRs often include templates that can help maintain consistency and accuracy in your notes.
Tips for Effective Documentation in EHR Systems
When using EHR systems, take advantage of any available templates to ensure consistency. Keep your notes organized and easily searchable, and ensure that all required information is included. Regularly review and update your notes to keep them accurate and relevant.
Conclusion
SOAP notes are a vital tool in speech and language therapy, helping therapists document patient progress, set goals, and communicate effectively with other healthcare professionals. By following best practices and avoiding common pitfalls, you can ensure that your SOAP notes are accurate, informative, and useful in providing the best possible care for your patients.
FAQs
How do I start writing a SOAP note?
Begin by gathering all relevant information from the session. Start with the Subjective section, recording the patient’s or caregiver’s perspective, followed by Objective data, Assessment, and Plan.
How often should I update SOAP notes?
SOAP notes should be updated after every therapy session to ensure that all relevant information is documented and any changes in the patient’s condition are recorded.
Can SOAP notes be used in other types of therapy?
Yes, SOAP notes are used across various medical fields, including physical therapy, occupational therapy, and counseling, to document patient progress and treatment plans.
What happens if I don’t write SOAP notes correctly?
Improper documentation can lead to legal issues, including audits, disputes, or claims of inadequate care. Accurate and thorough SOAP notes provide legal protection and demonstrate compliance with professional standards.
How can I improve my SOAP notes over time?
Regularly review your notes and seek feedback from colleagues. Practice writing clear, concise, and well-organized notes, and stay updated on best practices in documentation.



Hello fans of humor!
Basketball play on words that drive to the hoop with humor. basketball love puns Don’t foul out—these puns are all net.
Basketball love puns that are total relationship goals. For couples who know love is a team sport.
Toda la información en el enlace – п»їhttps://basketballpuns.com/
Wishing you lots of giggles!
?Hola exploradores del casino
Aprovecha los 20 euros gratis retirables para empezar a jugar y retirar tus ganancias sin complicaciones en los mejores casino online.
Ofertas actuales: Casino 20 euros gratis sin depГіsito – casino 20 euros gratis sin depósito
?Que tengas excelentes tiradas afortunadas !
?Hola entusiastas de las apuestas
Las casas de apuestas sin verificaciГіn tienen una ventaja clara sobre las reguladas: no te obligan a justificar tus ingresos ni controlar tus movimientos. Juegas lo que quieres, cuando quieres.
apuestas deportivas sin dni sin registro – apuestas online sin registro
?Que tengas excelentes momentos únicos !
?Hola participantes del casino
Marca casino 20 euros gratis ofrece bonos irresistibles para nuevos jugadores en EspaГ±a.
Casino sin depГіsito: Juega con 20 euros gratis ahora – casino 20 euros gratis sin depósito
?Que tengas excelentes juegos !